Get Inspired
Upcoming Events

The Wilful
20 Apr 2024

Bespoke Wedding Appointments
20 Apr 2024

Four Seasons Hotel Carlingford Exclusive Wedding Open Day this Sunday!
21 Apr 2024

Wedding Showcase
21 Apr 2024

Chat with Trisha at the Fabulous Annual Farnham Spring Wedding Showcase
21 Apr 2024

Wedding Showcase
21 Apr 2024

Wedding Open Day
21 Apr 2024

Wedding Showcase Afternoon
21 Apr 2024

Bentley Boys Livestream Showcae
23 Apr 2024

April Wedding Open Evening at Oriel House Hotel
25 Apr 2024
<
>
Current Competitions

WIN Afternoon Tea at Award Winning Barberstown Castle
8 Apr to 22 Apr 2024

WIN a romantic stay in The Hillgrove Hotel with dinner and spa treatments
1 Apr to 15 Apr 2024

WIN A Luxury Stay At Radisson Blu St. Helen’s Hotel
25 Mar to 1 Apr 2024

WIN a Romantic 2 Night Stay with Dinner at the McWilliam Park Hotel
19 Mar to 27 Mar 2024

Win a romantic stay at Thomas Prior Hall at Clayton Hotel Ballsbridge with dinner and wine
4 Mar to 18 Mar 2024
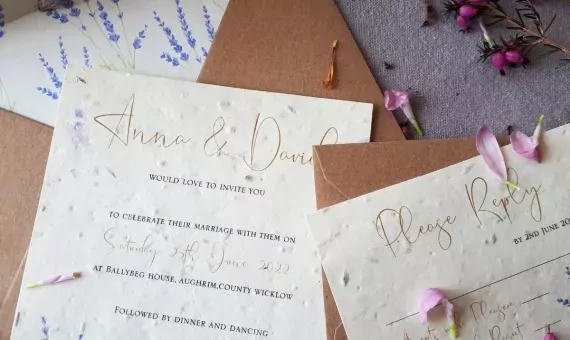
Win a €150 voucher for wedding invitations from Coill Design
4 Mar to 18 Mar 2024

WIN A Romantic Stay In Bridge House Hotel's Bridal Suite with Dinner
26 Feb to 4 Mar 2024

WIN a luxury stay at Dunboyne Castle Hotel & Spa
19 Feb to 26 Feb 2024

WIN 2 tickets for The Connor Mc Keon Band at The National Concert Hall
12 Feb to 26 Feb 2024

WIN The ICON Photo & Video Booth for your wedding from EntertainYou.ie
19 Feb to 26 Feb 2024
<
>
Are you sure?
This action cannot be undone













